Back in 2013 when I published the results of my testosterone-boosting experiment, I got chided by many commenters for recommending a diet high in cholesterol and fat. According to them, I was promoting a dangerous diet that would lead to heart disease and obesity, despite the fact that I also published the results of my blood test which showed stellar cholesterol numbers.
I don’t blame these guys for their criticisms. Like me, most of them probably grew up during the 80s and 90s when it was an article of faith that diets high in cholesterol and fat would result in heart disease and other health problems.
But everything most everyone knew about cholesterol has turned out to be wrong. (And that includes me and what I thought was a conclusive link between this lipid molecule and testosterone!)
In truth, cholesterol isn’t a bad guy. He’s just misunderstood. And today we’re going to share everything you need to know about Mr. Cholesterol and offer the real dope on this right old molecular chap.
The Benefits of Cholesterol
Without cholesterol, you would die.
Simple as that.
That’s because cholesterol is the raw material your body uses for a whole host of functions. For example, did you know that the membrane of all your cells consists of a good amount of cholesterol? Without it, we’d be gelatinous blobs because our cells wouldn’t have any structure to them.
Besides keeping us from melting into puddles of goop, cholesterol also provides the following benefits:
Sex hormones are made from cholesterol. Testosterone — the hormone that puts hair on your chest and makes you strong like bull — is made from cholesterol. And it’s not just T. Estrogen, and the sex hormones needed for female sex traits, are made from cholesterol, too.
Because cholesterol is a precursor to testosterone, a common side effect found among men taking statins (cholesterol-lowering drugs) is a drop in libido as well as an increase in erectile dysfunction. Several studies have confirmed the connection between lowered cholesterol levels and lowered testosterone levels.
So is the inverse also true? Will increasing your cholesterol consumption increase your testosterone levels? During my testosterone-boosting experiment, I assumed the answer was yes, which is why I wolfed down eggs and red meat for three months. However, after researching more, I haven’t been able to find a single study on whether or not increasing dietary cholesterol will indeed increase T levels, which is truly surprising. Researchers know that the Leydig cells in your testicles — the cells that create testosterone — have extra cholesterol requirements compared to other cells. Yet where they get that extra cholesterol isn’t entirely clear. Leydig cells can create their own cholesterol for testosterone when overall levels are down; however, when Leydig cells are forced to do so, T levels begin to drop. So perhaps dietary cholesterol fills the gap? (Note: one study has shown that olive oil allows Leydig cells to absorb more cholesterol, thus resulting in increased T levels. Be generous with that olive oil on your salad!)
Tim Ferriss experimented with increasing his T levels by ingesting large amounts of cholesterol — in the form of a shake made from whole milk and four raw eggs — right before he went to sleep. His personal experiment resulted in increased T levels in the mornings after he had drunk the shake compared to the mornings when he hadn’t. Yes, it’s an n+1 experiment and doesn’t have the authority of more rigorous studies, but it’s an interesting result to consider.
Bottom line: increasing dietary cholesterol may or may not increase T levels. (If you know of a study that has looked at that question, I’d love to hear about it!) But regardless of whether or not it does, eating a diet low in processed carbs and high in protein, which is also a typical byproduct of trying to ingest more cholesterol, may have other health benefits. This includes weight loss and muscle gain — effects which do conclusively raise your T.
Vitamin D is made from cholesterol. “Vitamin D” is actually a misnomer because it’s not a vitamin, but rather a hormone. And just as cholesterol serves as the precursor to sex hormones, it’s also necessary to the production of the hormone Vitamin D. Whenever the cholesterol in your skin is exposed to sunlight, particularly UV-B rays, a chemical reaction occurs which results in the production of Vitamin D3. Sure, you can take an oral supplement to get the same result, but if your body can make it free from just cholesterol and sunlight, you might as well take advantage of it.
Our bodies use Vitamin D for a variety of important functions such as immune response, regulation of calcium and phosphate, inflammation reduction, and even gene expression. Increased levels of it are associated with better mental and emotional health as well as increased testosterone levels.
So what are you waiting for? Put that cholesterol to use by catching some rays.
Bile acids are made from cholesterol. That steak you ate last night had to be broken down so your body could use it for nutrients. Bile acids play an important role in that breakdown process. And yep, bile acids are made from our handy friend, Mr. Cholesterol.
Cholesterol is vital for brain health. Your brain is filled with cholesterol. Not only does your noodle use it to make new neural cells, it’s also used to maintain their integrity and facilitate cellular communication by helping form the myelin sheaths that coat the cells.
Studies have found that low cholesterol levels (around 160 mg/dL or less) are linked to memory loss, depression, and aggression. Research has shown that cholesterol may play a role in the effective release of neurotransmitters; without it, your brain just can’t make all the cellular connections it needs to maintain its sharpness and vibrancy.
If you’re looking for a quick way to up your cholesterol intake to maintain a healthy brain, eat the brains of other animals. No, really. Apparently noshing on squirrel brains mixed with scrambled eggs is a thing. That’s a cholesterol mega-dose right there.
Cholesterol may help fight infections. Research has shown an inverse correlation between cholesterol levels and infections — the lower your cholesterol levels, the greater your vulnerability to getting sick. So how does cholesterol fight infections? Studies suggest that LDL (the so-called “bad” cholesterol — more on LDL below) plays a role in stimulating our immune system to fight off infection. When cholesterol levels are low, there’s a decrease in the production of certain antibodies.
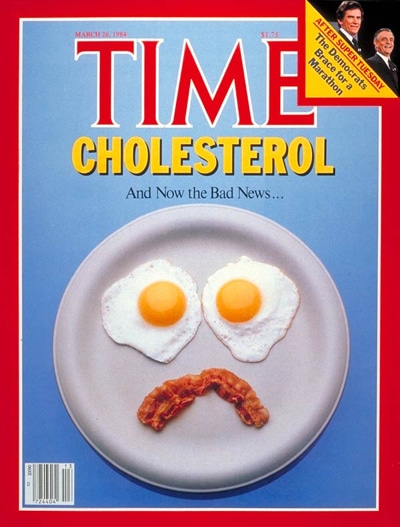
Why Cholesterol Got a Bad Rap
If cholesterol provides so many health benefits, how did it get such a bad rap?
It was a mixture of bad science and politics as usual.
Back in the 1950s, Ancel Keys, the scientist who created the K-ration for WWII soldiers, noticed that well-fed American business executives had high rates of heart disease, while malnourished individuals living in post-war Europe had lower rates of it. Keys hypothesized that the American diet — which was filled with high fat, high cholesterol foods — was responsible, and he concocted a study to prove it.
His famous “Seven Countries” study was one of the first longitudinal studies to test the effect of diet on health. Keys examined saturated fat and cholesterol consumption in seven countries (hence the name) and found a seemingly perfect relationship between rates of heart disease and rates of cholesterol and saturated fat consumption. His data showed exactly what he had predicted it would.
Right away, other researchers questioned the validity of the study. A British doctor named John Yudkin was particularly skeptical. Yudkin had done similar research and found several countries that had above average intake of saturated fat consumption but low rates of heart disease. Yudkin, along with other scientists, basically accused Keys of cherry-picking the countries in his study in order to prove his conclusion. They argued that it wasn’t cholesterol and fat that caused heart disease, but rather increased sugar consumption that was the true culprit.
But because of Keys’ role in developing nutrition standards for soldiers during WWII, he had tremendous political clout with congressmen, agency bureaucrats, and the media. Encouraged by the results of his study, Keys began to lobby heavily for the U.S. government to recommend low fat, low cholesterol diets. In 1977, Senator George McGovern, the chairman of the Senate Select Committee on Nutrition and Human Needs, published dietary guidelines based on Keys’ research that would radically change how Americans ate. The guidelines called for a diet low in fat and cholesterol and high in carbohydrates from vegetables and grains. The USDA issued guidelines recommending only 300 mg of dietary cholesterol a day. Which isn’t very much. Just two whole eggs contain 374 mg of cholesterol.
The result was a boom in food products marketed as “Low Fat” and “Heart Healthy.” Low-fat Snackwell cookies, cholesterol-free margarine, and non-fat potato chips lined the shelves of grocery stores. Americans replaced natural foods that had been common fare for centuries with these lab-produced, factory-made products. They stopped eating eggs and butter, switched from whole to skim milk, and gave up on bacon.
What’s more, pharmaceutical companies jumped on this bandwagon and created cholesterol-lowering drugs called statins. Statins work by blocking a substance your body needs to create cholesterol. Doctors began prescribing these drugs by the boatloads to any patient who walked in with higher than normal cholesterol levels.
But a funny thing happened.
Despite the fact that more Americans were eating low-fat and cholesterol-free foods, heart disease rates and obesity continued to climb. What gives?
Well, come to find out Yudkin and his colleagues were right. It wasn’t cholesterol and fat that caused people to gain weight and get heart disease; it was sugar and processed carbs. And guess what food manufacturers often replaced the missing fat with in their “heart healthy foods”? Sugar and processed carbs, of course. And that cholesterol-free margarine? It was made from hydrogenated vegetable oil that created trans fat, a type of fat that actually is linked to heart disease and stroke.
Those supposedly heart-healthy diet guidelines from the 70s were wreaking havoc on the circulatory systems of tens of millions of Americans.
And all those statin prescriptions? They worked wonderfully at lowering cholesterol…but probably a little too wonderfully. Many patients began complaining about symptoms like memory loss, depression, increased infections, erectile dysfunction, and lowered testosterone levels. Researchers discovered that in many patients, statins lowered cholesterol levels so much that the body wasn’t getting enough of the cholesterol it needed for healthy functioning.
Thankfully, in the past few years, we’ve regained some sanity when it comes to fat and cholesterol. Recent research has confirmed what scientists 60 years ago knew. It’s not dietary cholesterol and saturated fat that causes heart disease, it’s sugar combined with other lifestyle factors — like stress and being sedentary — that promote inflammation.
Consequently, government agencies and health organizations are backtracking on their stringent dietary cholesterol limits. In fact, earlier this year, the Dietary Guidelines Advisory Committee issued a draft document stating that dietary cholesterol plays little or no role in heart disease and that most folks probably shouldn’t worry about how much cholesterol they’re eating. While the panel doesn’t issue official guidelines, agencies responsible for food guidelines usually adhere very closely to them.
When it comes to statin prescriptions, many doctors are now using much more discretion. Instead of prescribing them to anyone with above average cholesterol levels, doctors now only do so for high-risk heart disease patients. Who’s a high-risk patient? Basically, those who already have existing heart disease.
How Your Body Gets the Cholesterol It Needs
Your body produces about 80% of the cholesterol it needs during the day; the other 20% comes from food.
About 20% to 25% of the cholesterol that your body produces is created in the liver from fatty acids. Other places where your body manufactures cholesterol include your intestines, adrenal glands, and reproductive organs.
When you consume foods with cholesterol, your body uses it. If you consume a lot of cholesterol, your body will just decrease the amount that it produces itself. If you don’t consume much cholesterol, your body will simply increase the amount it produces on its own. So even if you eat all the bacon and eggs you can stomach (like I do), your overall cholesterol levels will probably stay about the same (as mine have).
Genetics, not diet, seems to play a larger role in your overall cholesterol levels.
Beyond Good and Bad Cholesterol: HDL and LDL Cholesterol
Cholesterol is transported in the blood attached to carrier proteins. These cholesterol-protein combos are called lipoproteins. Lipoproteins are typically broken up into two groups based on their density: high-density lipoproteins (HDL) and low-density lipoproteins (LDL).
For years, researchers and doctors have called HDL “good cholesterol” and LDL “bad cholesterol.” While that’s roughly accurate, recent research has given us a much more nuanced look at HDL and LDL cholesterol. For example, not all HDL is good and not all LDL is bad. Below, we break down everything you need to know about these two groups.
HDL Cholesterol. The reason doctors call HDL “good cholesterol” is because HDL removes the so-called bad LDL cholesterol from the body. HDL does this by transporting cholesterol away from the body’s tissues and back to the liver where it’s turned into bile and excreted out of your body. HDL is what gets rid of excess cholesterol in your body and prevents build-up in your arteries.
Because HDL is your body’s cholesterol garbage truck, the more you have, the better. Recent research suggests that your HDL should be more than 60 mg/dL.
While HDL as a broad category is good for you, recent research has shown that not all HDL is the same. There are two subtypes; one is good for you, the other not so much. HDL-2 particles are large, buoyant, and provide the most protection from the build-up of LDL cholesterol. These particles are also anti-inflammatory. HDL-3, on the other hand, is small, dense, and possibly inflammatory. So while you want a high overall HDL number, you’ll want to have more HDL-2 than HDL-3 in your system. Newer tests can suss out the difference between the two, and researchers are developing therapies to target lowering just HDL-3. However, for most folks, you don’t need to worry too much about the two sub-types. Just knowing your overall HDL will do.
To increase your HDL levels, get plenty of exercise, don’t smoke, and increase your consumption of healthy monosaturated fats that you’ll find in foods like olive oil, avocados, fish, and nuts.
LDL Cholesterol. LDL is considered “bad” cholesterol because it can build up in the arteries, blocking blood flow. Unlike HDL that transports cholesterol away from body tissue and to the liver, LDL delivers cholesterol to the body after the liver produces it.
While our body needs the cholesterol that LDL delivers, too much of it could create health problems by building up in the arteries. Consequently, researchers and doctors recommend that folks shoot for an LDL that’s lower than 100 mg/dL.
Just as with HDL, not all LDL is the same. There are two types of LDL particles. One is terrible for you and the other only causes problems when it’s oxidized. LDL-A is a big, fluffy molecule that won’t cause any harm to your system so long as it’s not damaged by oxidation, which occurs when free radicals attach to the LDL. When this happens, the cholesterol converts to plaque. Researchers believe LDL-A levels play little or no role in heart disease or other circulatory problems.
LDL-B, on the other hand, is the bad kind. It’s a small, hard, and dense molecule that causes your arteries to harden. While you should focus on lowering your overall LDL levels, you’re better off having more LDL-A and less LDL-B. Blood tests can measure both of these.
To lower your LDL levels, get rid of excess body fat and increase your HDL levels with the lifestyle suggestions above. Research has shown that increased consumption of saturated fat can help decrease the amount of LDL-B particles in your system.
Lp(a): The Alpha Wolf Cholesterol Particle. While HDL and LDL levels get the lion’s share of attention, there’s a third type of lipoprotein that likely has more of an influence on your risk for heart disease than both HDL and LDL levels. Lipoprotein(a), or Lp(a), is a very small, yet highly inflammatory particle that promotes the blood clotting that can lead to coronary heart disease and stroke. Lp(a) is so patently bad for you, cholesterol expert Dr. Stephen Sinatra calls it the “alpha wolf cholesterol particle.”
Lp(a) isn’t a problem in low amounts. In fact, it serves a useful purpose in that it helps repair and restore damaged blood vessels. The problems start whenever your body has to use Lp(a) frequently to perform this function, as often happens when folks have chronic inflammation.
Most cholesterol blood tests don’t measure Lp(a) levels so if you want to know yours, you’ll have to ask for a test that specifically measures it. Ideally Lp(a) levels should stay below 30 mg/dL. Lp(a) levels are primarily determined by genetics, so if you have a family history of early arterial diseases, you should get your Lp(a) levels checked.
The current recommended treatment for high levels of Lp(a) is 1-3 grams daily of niacin, also known as Vitamin B3. When you take niacin at such high levels, you’ll experience what’s called a “niacin flush,” a harmless yet uncomfortable reddening and warming of your skin. To manage the flush, start off your niacin supplementation at 100 mg and very slowly increase the dosage.
Give It to Me Straight Doc: Is It Okay to Eat Cholesterol?
First, I’m not a doctor, I just play one on TV. And by TV I mean online.
With that said, based on my research on the current studies out there about cholesterol, most folks can wolf down Ron Swanson-amounts of cholesterol without increasing their levels or putting themselves at risk for heart disease. A very small percentage of the population has genes that cause their cholesterol levels to rise significantly when they eat diets high in it. These folks will need to watch their cholesterol intake. To find out if you’re what scientists call “hyper-responsive” to cholesterol, you’ll need to take a test with your doctor.
What goes for cholesterol goes for fat as well. Research has found little connection between heart disease and fat — both the saturated and unsaturated varieties. You do want to stay away from trans fat, though. That’s the man-made fat that has been shown to cause heart disease and other circulatory problems. Keep your foods as whole and natural as possible.
Now you know there’s no need to keep old Mr. Cholesterol at arm’s length. Invite him in for a bacon and egg breakfast and tip your hat to his brain-boosting, infection-fighting, possibly T-raising ways.
Want to share your thoughts on this article? Send us a tweet or join the discussion on Facebook!